For centuries, Mother Nature has been the inspiration for new and innovative medical treatments. One of the more unlikely inspirations in recent years—with potential use in treating inflammatory and autoimmune diseases—involves one of the natural world’s least-celebrated liquids: the saliva of a tick. To understand how a tick’s spit could potentially advance medicine, let’s first take a step back.
For centuries, Mother Nature has been the inspiration for new and innovative medical treatments. One of the more unlikely inspirations in recent years—with potential use in treating inflammatory and autoimmune diseases—involves one of the natural world’s least-celebrated liquids: the saliva of a tick. To understand how a tick’s spit could potentially advance medicine, let’s first take a step back.
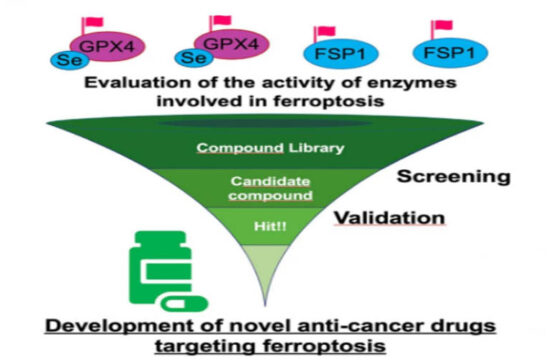
It is important to begin by noting that acute or chronic inflammation is a common component of many clinical disorders. In recent years, the complement system has been linked to a growing number of inflammatory and immunological conditions, and it is believed that excessive activation or insufficient control of complement activation on host cells can cause an immune imbalance.
This, in turn, may fuel a vicious cycle between complement, inflammatory cells and tissue damage that exacerbates clinical complications (Ricklin D and Lambris JD, The Journal of Immunology, 2013, 190:3831-3838). Although the exact involvement of complement needs to be carefully investigated for each disease, the therapeutic modulation of complement activity has emerged as an attractive target for the inhibition of inflammatory and immune processes.
[pullquote]Positive interim data have been obtained from a Phase 1b study demonstrating sustained complement inhibition using once-daily subcutaneous maintenance dosing with Coversin.[/pullquote]
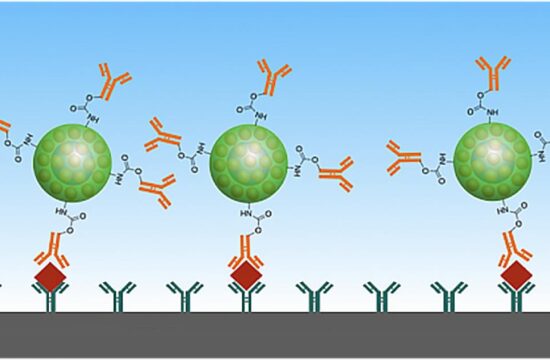
It is particularly fruitful to study the protein C5, which ordinarily splits into two components in the complement system to clear out foreign invaders and unwanted cells. In complement dysregulation, the C5 components are produced triggering inflammatory and autoimmune conditions.
A novel form of treatment, called C5 inhibition, involves medications that bind to C5 and prevent runaway formation of its two components. An FDA-approved C5 inhibitor, the antibody Soliris (eculizumab), has been on the market since 2007. However, concerns have been raised regarding its cost and the need for intravenous administration at two-week intervals.
A new C5 inhibitor, a small recombinant compact protein named Coversin, has been derived from a protein in the saliva of the Ornithodoros moubata tick. The natural Coversin molecule works by damping down the immune response of the host animal that the tick feeds off of, enabling the tick to repeatedly feed without damage from host inflammatory substances.
Given by subcutaneous injection, Coversin makes once-daily self-administration possible and avoids IV infusion altogether. Although it binds to C5 in a different location than eculizumab, data so far indicate Coversin acts on C5 in the same way. Although conceived as a first-line therapy due to its route of administration, it has also shown it may help patients who are resistant to eculizumab. Positive interim data have been obtained from a Phase 1b study demonstrating sustained complement inhibition using once-daily subcutaneous maintenance dosing with Coversin.
Coversin has shown 100 percent inhibition of complement C5 activity within 12 hours in a Phase 1a study in humans. It has also demonstrated the ability to achieve full complement inhibition in the blood of eculizumab-resistant patients, offering a potential alternative to those for whom eculizumab is ineffective. Plans are underway to study Coversin for compassionate use in those patient populations that exhibit eculizumab resistance.
The initial clinical targets for Coversin include the rare disease paroxysmal nocturnal hemoglobinuria (PNH). PNH patients exhibit blood cells lacking the gene PIG-A; without it, key proteins fail to connect to the cell surface and do not protect the cell from the complement system. As a result, red blood cells break down too early. The current standard of care comprises steroids, blood transfusions and blood thinners. Although eculizumab is indicated for PNH, Coversin’s self-administration may present a more convenient alternative. Beginning in February 2016, a PNH patient has been treated with Coversin with good response, and a Phase II study has been initiated.
Another Coversin target is atypical hemolytic uremic syndrome (aHUS), which is also an approved indication of eculizumab and causes abnormal blood clots to form in small blood vessels in the kidneys. If the complement system gets out of control, sometimes due to mutations in complement genes, sometimes due to autoantibodies or other reasons, patients can develop aHUS. A Phase 2 study in aHUS is expected to be initiated in late 2016.
A third potential Coversin target is Guillain-Barré syndrome, in which the immune system attacks part of the peripheral nervous system. The current standard of care involves treatment with intravenous immunoglobulin or plasma exchange, yet a small but significant percentage of those treated experience permanent impairment. There are plans to initiate a Phase II study in GBS patients in early 2017 and orphan drug designation has been assigned by the U.S. Food and Drug Administration as well as by the European Medicines Agency for use in the EU.
Coversin may also be applicable as a treatment for other diseases such as Sjögren’s syndrome, the inflammatory disease known for triggering dry eye and dry mouth along with other symptoms. In the autoimmune attack that causes Sjögren’s, disease-fighting white blood cells target glands that produce moisture—primarily the lacrimal and salivary glands. For the dry eye symptom, Coversin can be adapted into a topical ocular treatment, once again making self-administration possible. A 60-day topical eye toxicology study has been successfully completed and there is evidence Coversin has activity against eye surface inflammation.
Additional clinical studies are likely to clarify the potential role of Coversin within the toolkit of doctors who patients currently suffer from a range of inflammatory and autoimmune diseases. And to think—it all begins with the saliva of a tick.
Gur Roshwalb, M.D. is Chief Executive Officer of Akari Therapeutics, a clinical-stage biopharmaceutical company focused on the development and commercialization of innovative therapeutics to treat orphan autoimmune and inflammatory diseases.
Source: Drug Discovery and Development