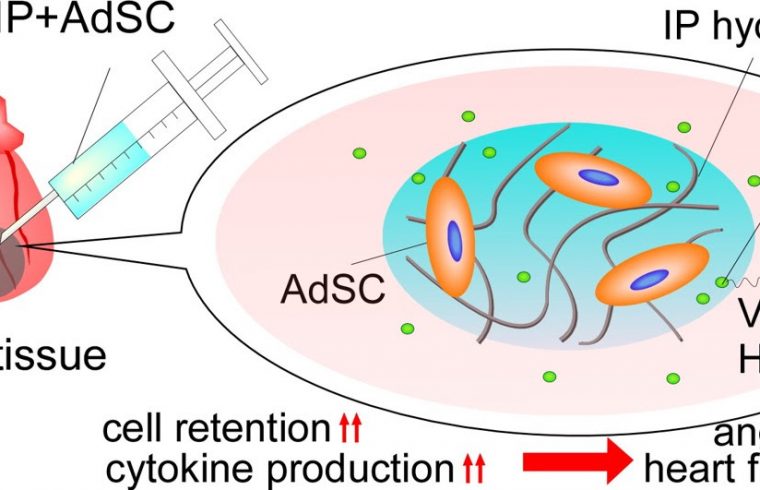
The hydrogel acts as a scaffold that holds the stem cells in place at the site of injection and keeps them alive for longer. The stem cells produce cytokines that stimulate the formation of blood vessels to help the heart recover. The gel is biodegradable, so it eventually dissolves and is removed by the body.
Heart muscle becomes damaged and cardiac function is affected when blood vessels feeding the heart are blocked. A new stem-cell-carrying hydrogel helps mice recover from this condition, called myocardial infarction, by stimulating formation of new blood vessels. Developed by a team of scientists at Kansai University in Japan, the stem cell delivery system is described in the journal Science and Technology of Advanced Materials.
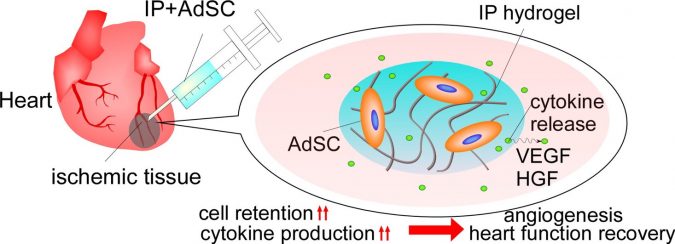
The team used stem cells derived from fat tissue in their application. These so-called ‘adipose-derived stem cells’ have already been investigated for treating damaged cardiac tissue from reduced blood flow to the heart, known as myocardial ischemia.
The idea is that the stem cells will release stimulating factors to regenerate blood vessels once injected into damaged heart tissue. The problem, though, is that they can’t be retained or survive in the tissue long enough. In other studies, scientists have found that injecting cell-free biodegradable hydrogels into damaged heart tissue helps partial recovery of heart functions.
Kansai University bioengineer Yuichi Ohya and his colleagues mixed the two techniques together.
Firstly, they developed hydrogel formulas that can hold stem cells in place for longer periods of time at the site of tissue damage. These hydrogels start off as a solution when they are at room temperature. This makes it easy to mix in the stem cells. When the solution is injected into an organ, it warms to body temperature, triggering its transformation into a gel.
One of their hydrogels was especially good at staying in its gel state. It was made with a combination of molecules, called tri-PCG, with acrolyl groups attached to them. The tri-PCG-acryl was then mixed with a polythiol derivative.
The team added adipose-derived stem cells to the hydrogel and observed, both in petri dishes and inside mouse heart tissue, how long the cells lived and what kinds of genes and substances were produced by the cells.
“The stem cells were able to survive in our injectable hydrogel and released molecules that stimulate blood vessel formation, improving heart function and making it effective for treatment of ischemic heart,” says Ohya.
The team next plans to test their therapy on larger animals after confirming its safety, and then to conduct clinical studies in humans. They also plan to investigate using their injectable hydrogel to deliver immune cells to treat cancer or in vaccines to protect against viral infections.