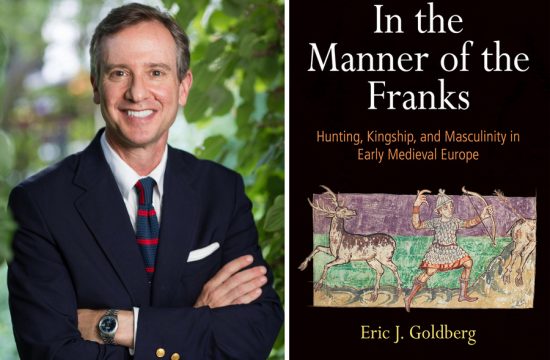
MADISON – At Joshua Medow’s first job, in the Neurocritical Intensive Care Unit at UW Hospital and Clinics, he saves lives. His patients have endured strokes, car accidents and shootings.
At his second job, he puts his engineering talents to work inventing devices to make his first job a bit easier, such as a new type of ventilator to help people breathe when their lungs are severely compromised.
A critical-care expert at the University of Wisconsin School of Medicine and Public Health, Medow has four medical accreditations, multiple teaching, doctoring and administrative responsibilities at the hospital and medical school, and that extracurricular inventor-entrepreneur habit.
Those qualifications may sound intimidating – but then Medow introduces himself simply as “Josh.” He’s equally down to earth during rounds in the neuro ICU, a UW hospital facility that he developed and directs, revealing a naughty practical joke from his past, explaining when a more expensive medical test can be justified, and gently making inquiries that move students’ narrow technical questions toward the jillion subjects on a future doctor’s “need to know” list.
All this while smiling, maintaining eye contact and putting down only himself.
Rounds prove to be a goulash of medical lingo, lab results and common sense:
Medow: “What would make you decide this patient is not ready to go home?”
Student: “Not having a home-care provider?”
Medow: “That could be an issue, but he’s plenty ‘with it.’ It just depends on what you are able to do.”

CREDIT: Jeff Miller/UW-Madison
The patient has had nasal surgery, and Medow finally offers up the symptom he’s driving at: A salty taste in the mouth and lots of postnasal drip would signify a “leak” in the membrane that contains the cerebral-spinal fluid that bathes the brain.
Even though Medow calls his process “beating on” students, it’s respectful and encouraging, not the grilling that reputedly dominates this rite of medical passage.
The approach worked, said Iowa native Nathan Baggett, a third-year medical student on rounds. “As we presented our patients, we were constantly interrupted with questions, asking us to explain a lab value, or why the patient was showing some finding. Often, he would turn it into a detailed explanation of the neurological, surgical or basic medical management issues.”
Medow “was so kind in his feedback, even when he was being harsh, or challenging you on something you did not know, it felt like it was from a good place,” Baggett says. “It was a growing opportunity for us.”
Medow, 41, grew up in Skokie, Illinois. His father was a Vietnam War veteran who, after returning home, found work as a hotel bellhop. “When the economy skidded in the ’70s, he started a junk auto parts business out of home while working two other jobs.”

Medow originally intended to pursue computer engineering, but while he was in high school, his cousin died of leukemia. “I decided to become an oncologist, but once I got into medical school, I did not like oncology all that much. I still liked computers, and I figured, what better computer than the human brain? So I chose neurosurgery.”
His father, he adds, “generally dislikes doctors. Becoming a physician was my last chance at rebellion.”
Medow came to Madison in 1999. He’s now an associate professor of neurosurgery and biomedical engineering. His board certifications include neurosurgery, neurocritical care and clinical informatics.
In his ICU rounds, Medow often refers to his “engineering” approach. For example, a breathing tube cannot be removed until the patient meets three specific criteria. But the decision also requires a judgment call: What else does the patient’s condition tell us?
[pullquote]A critical-care expert at the University of Wisconsin School of Medicine and Public Health, Medow has four medical accreditations, multiple teaching, doctoring and administrative responsibilities at the hospital and medical school, and that extracurricular inventor-entrepreneur habit.[/pullquote]
One recent outgrowth of that engineering aptitude is the Digital Intern, software Medow created that guides hospital staff by suggesting clinical decisions. The system has been tested on organ donors, where it allowed the retrieval of 25 percent more organs, combined with a 61 percent reduction in critical care hours billed – outcomes that translate into the saving of money and lives.
That idea grew from daily experience, Medow says. “If I’m trying to keep five patients going, and then I have an organ donor who is unfortunately not going to live, what do I do? This could save the lives of seven or eight other people. That was the necessity that was the mother of this invention.”
How does Medow deal with a job that puts him face to face with too much pain and sorrow?
“There’s a certain amount of denial, and a certain amount of ‘I can make it better,'” he explains. “I have the opportunity to help people who are critically ill due to shootings, car accidents and other tragedies. This job gives me a chance to give these people the best opportunity for a meaningful quality of life. If I thought I could not make it better, I’d be too depressed to go to work, but so many of our patients do get better.”
One patient who is getting better is a young boy who was shot in the head in southwest Wisconsin in January. Critically injured, he was placed in an induced coma at the American Family Children’s Hospital, where Medow treated him.
The top post on a public Facebook page records the family’s gratitude: “What a transformation … Thank you for taking a chance that night on Joey when others may have thought it was a lost cause. He is truly here because you cared.”