Researchers from the Johns Hopkins Kimmel Cancer Center have created a system to study an aggressive subtype of medulloblastoma, which is a rare pediatric brain tumor that generally has a very poor prognosis.
While more than 60 percent of children with medulloblastoma can be effectively treated, one subtype of the disease, known as Group 3 medulloblastoma, has a survival rate of less than a few years after diagnosis.
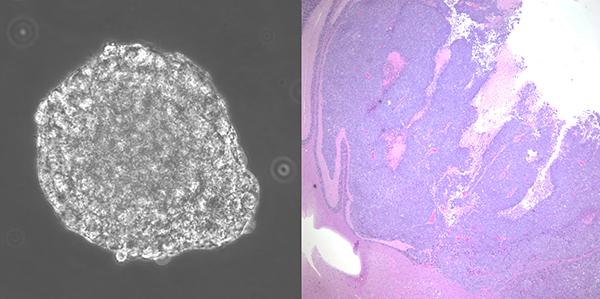
Genetically accurate laboratory models of Group 3 medulloblastoma were difficult to come by, so the researchers decided to engineer human neural stem cells to create a new model of medulloblastoma. Using genetically engineered viruses, the scientists replaced copies of the normal genes with mutated copies of MYC, TP53, hTERT, and AKT, which are thought to drive this specific subtype of the disease.
They injected the engineered stem cells into mice brains and aggressive tumors developed and spread through the body in a similar way as seen in patients. The tumors continued to express the mutated genes and about 20 percent of the tumors spread to the spine, which is often seen in Group 3 tumors.
[pullquote]After testing the drug in the new mouse models of Group 3 medulloblastoma, the team found the CDK inhibitor extended median survival of the mice by almost 50 percent.[/pullquote]
The team, led by Eric Raabe, M.D., Ph.D., a pediatric oncologists at Johns Hopkins, then used a computer algorithm known as Disease-model Signature vs. Compound-Variety Enriched Response (DiSCoVER), to help identify drugs that may be effective against the disease.
The tool matches the engineered cells’ genetic profile with profiles of hundreds of cancer cell lines in a large database. The system anticipated that a class of drugs known as cyclin-dependent kinase (CDK) inhibitors might do the trick. Through the database they found and tested one of these drugs, palbociclib (Ibrance), which is approved to treat metastatic breast cancer.
Using the tool, “we could figure out which cell lines were most closely related to our neural stem-cell model of medulloblastoma, and then use that information to predict which drugs might also be active in this model,” Raabe explained in a prepared statement.
After testing the drug in the new mouse models of Group 3 medulloblastoma, the team found the CDK inhibitor extended median survival of the mice by almost 50 percent. Their survival increased from 25 to 37 days. The drug successfully crossed the blood-brain barrier, entered the tumor and prevented further tumor cell growth.
The findings could have implications for other types of cancer as well, according to Raabe. CDK inhibitors may be included in a clinical trial that is presently being planned by the Children’s Oncology GroupExit Disclaimer, for patients with relapsed medulloblastoma, based on this study and others that have yet to be published.
“We’ve used pediatric cancer as a model because we’re pediatric oncologists, but we think this could be done with other cancer types as well,” Raabe said.
Currently Raabe and his colleagues are testing their system to create a new model of another subtype of medulloblastoma.
The findings were published Aug. 1 in Clinical Cancer Research.