New research shows that mixing low viscosity alginic acid with calcium phosphate cement (CPC), a material commonly used as a bone replacement, confers 3 functional improvements: shorter setting time, increased compressive strength, and acquisition of porosity.
One reason for the increased use of CPC in recent years is its self-setting nature, allowing it to be injected into a patient for a more non-invasive approach. However, CPCs have a dense microstructure that make it difficult for cells to enter. This lack of pores limits the potential for new bone growth. This study, published in the Journal of Materials Science: Materials in Medicine, explores the effect the naturally derived biopolymer alginic acid has on this issue.
Previous research has studied other biopolymers, including gelatin, collagen, and chitosan, but this joint study between the Osaka City University (OCU), Graduate School of Medicine and Graduate School of Engineering, has confirmed the positive effects of mixing alginic acid with CPC.
In vitro studies showed alginic acid shorten setting time and increase compressive strength of CPC. In addition, in vivo studies showed the biopolymer increase porosity of CPC, allowing cells to enter and new bone to grow.
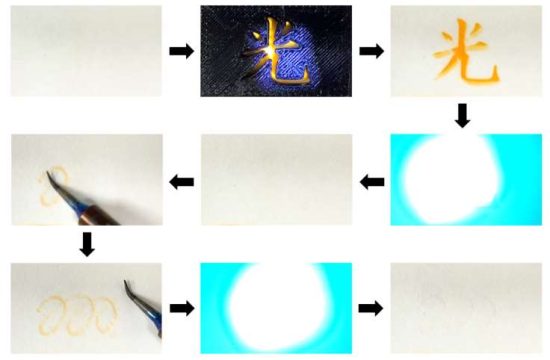
Alginic acid has been widely used in the medical field for procedures such as, cell immobilization, drug delivery, and wound dressing. However, there have been limited studies in conjunction with CPC. The degradability and cross-linking characteristics of alginic acid make it a promising additive to improve on the dense and generally poor mechanical properties of CPC.
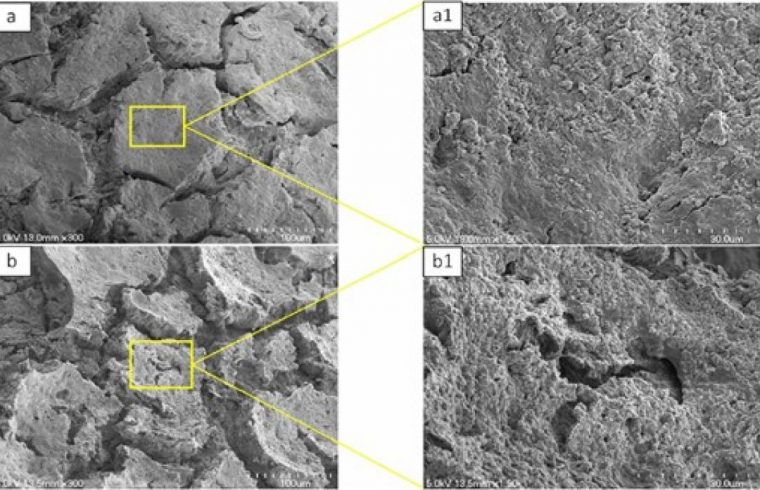
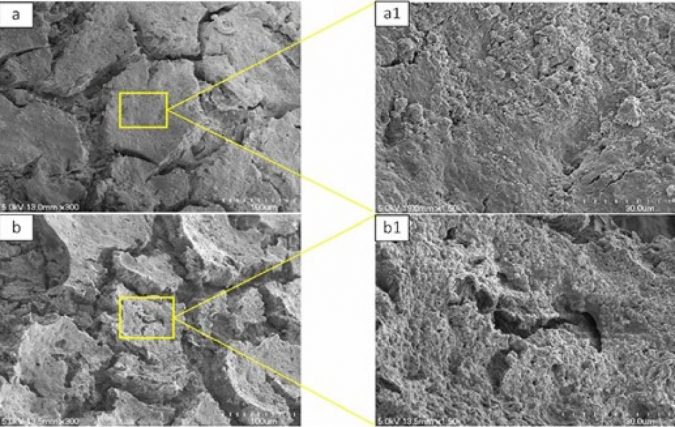
This new study evaluated a series of CPC-alginate (the salt form of alginic acid) compounds with increasing amounts of alginic acid. In vitro, a pH meter showed a decrease in pH levels as alginic acid amounts increased, speeding up setting time. Scanning electron microscopy revealedthat compounds with increased alginic acid had more pores and less density. In vivo, X-ray and micro-CT analysis showed that femurs injected with CPC compounds of increased amounts of alginic acid had, after 6 weeks, more degradation and bone formation than the control group.
“Artificial bones can support broken bones, but they do not replace our own bones and remain in the body as a foreign object” said Graduate Student Akiyoshi Shimatani, and first author of the study. Associate Professor Hiromitsu Toyoda of the OCU Dept. of Orthopedic Surgery continued: “To solve this problem, we have developed an artificial bone in collaboration Professor Yoshiyuki Yokogawa and his team from the OCU Faculty of Engineering, which is sticky, hard to break, and replaces the body’s own bone. We hope this becomes a new option for artificial bones.”