Clinical-stage immuno-oncology company TapImmune Inc., is on the quest to beat down ovarian and breast cancer using vaccines that target T-cells on two fronts.
Clinical-stage immuno-oncology company TapImmune Inc., is on the quest to beat down ovarian and breast cancer using vaccines that target T-cells on two fronts.
The Jackson, Fla.-based company started over 10 years ago, but didn’t begin its foray into cancer treatments until CEO Glynn Wilson took over several years ago.
President and COO John Bonfiglio spoke with Bioscience Technology to discuss the company’s technology and upcoming clinical trials.
Bonfiglio started as a consultant to TapImmune in 2015, but has in the biotech business for over 27 years, running small companies as CEO and helping to both raise money and refocus the business on technology.
TapImmune currently has three therapies in development called TPIV 200, TPIV 110 and TPIV 100.
The T-cell vaccine technology was invented by Dr. Keith Knutson at the Mayo Clinic, where TapImmune licensed it from, and it involves therapies that are derived from actual cancer patients, not from animal models. Knutson is also an advisor to the company.
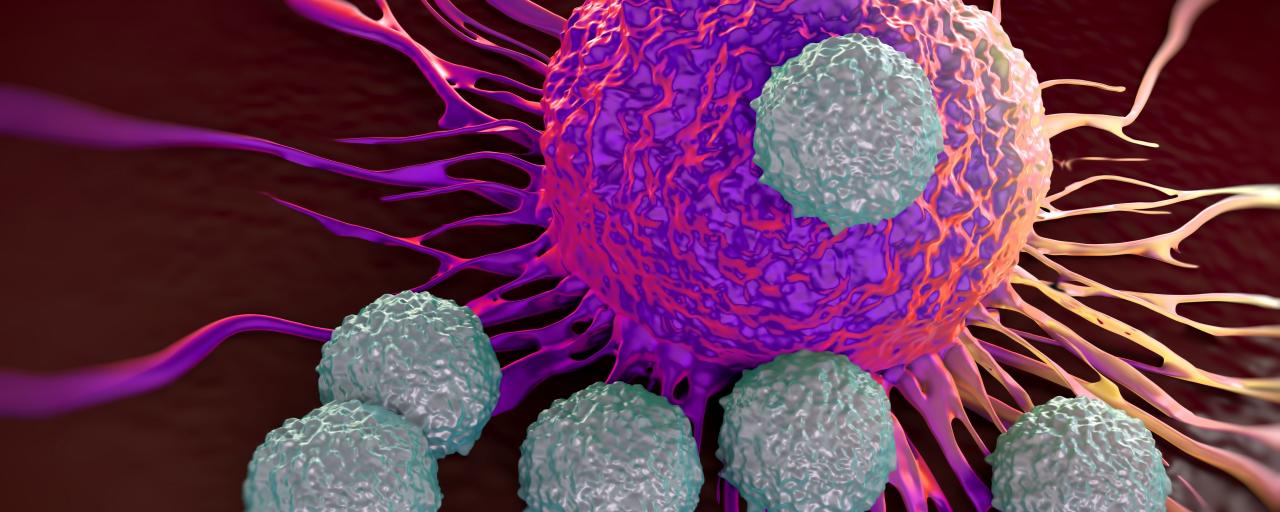
Unlike some treatments which only target killer T-cells (CD8) cells, TapImmune’s vaccines stimulate both killer T-cells and helper T-cells.
“In the recent 5-10 years people have come to understand that killer T-cells are a small component of person’s immune system,” Bonfiglio said. “About 75 percent of the T-cells are helper T-cells.”
He explained that these need to be activated alongside the CD8 cells, because they can turn into both killer T-cells and memory T-cells, which can stick around and help prevent metastatic disease.
Bonfiglio compared it to a polio or tetanus vaccine that requires memory within in the immune system, so that anytime a person come across the disease the immune system recognizes it and is able to kill it right away.
TapImmune’s vaccines are being tested in three separate clinical trials.
One is sponsored by the Mayo Clinic, with a $13.3 million grant from the Department of Defense, designed with TapImmune protocol. It’s a 280 patient, double-blind, placebo controlled study, using TPIV 200 as a standalone agent for triple negative breast cancer. The study is completely under the control of the May Clinic and Department of Defense, Bonfiglio said, but the company will have access to the data once it’s generated.
Enrollment in the trial is scheduled to start this quarter, but could be as late as first quarter next year Bonfiglio said.
A second study will see how TPIV 200 works in combination with AstraZeneca’s checkpoint inhibitor, durvalumab, in patients with ovarian cancer who have failed chemotherapy and have few options for treatment.
Bonfiglio sees combination therapies as the future of cancer treatment. He noted that Merck alone has 250 or so ongoing trials with their checkpoint inhibitor Keytruda, and that most of those are in combination with some other form of therapy.
“”People realize the immune system is so complex that you need to attack it from several different angles,” Bonfiglio said.
The checkpoint inhibitors as designed to prevent cancer cells from sending out a signal to the immune system to shut it down so it doesn’t activate against the cancer cells, while TapImmune’s drug enhances the immune system to increase the number of T-cells, which Bonfiglio said are essentially “the point of the spear” attacking cancer cells.
“On one hand you have something that’s taking the breaks off of the immune system, and on the other hand you have our product which is enhancing the immune system, so it’s a natural fit from a scientific standpoint.”
The trial, taking place at Memorial Sloan Kettering, is a 40-patient open label, double blind trial. Both AstraZeneca and TapImmune are providing their respective drugs, and funding for half the cost of the trial each. The goal is to control the regulatory T-cells in ovarian cancer.
TapImmune received Fast Track Approval and Orphan Drug Status from the Food and Drug Administration (FDA). Fast Track Approval was granted for TPIV 200 used in ovarian cancer patients who are responding to platinum therapy. It will be used in combination with chemo to hopefully keep patients from recurring for longer periods of time, Bonfiglio said.
The company is sponsoring a small trial that should have 12 sites enrolled by the end of the year.
One benefit of having Fast Track Approval is that the company can have frequent communication with the FDA and the option of submitting pieces of the NDA in real time, saving time, Bonfiglio said.
He also noted that Orphan Drug Status is great because it gives the company seven years of exclusivity.
In addition to the cancer vaccines, the company has also developed technology, known as PolyStart, designed to be a platform for DNA vaccines.
With a DNA vaccine, you take DNA, make a protein, and put that into cells in a patient, and then the patient’s cells make the protein to induce an immune response, Bonfiglio explained.
Usually if you have one DMA molecule, it converts to one messenger RNA molecule, which converts to one protein. However, if you take one PolyStart molecule and put it into a cell, it can convert it into four or more proteins, rather than just one, according to Bonfiglio.
“The more proteins you produce, the more likely you are to have a very large immune response,” Bonfiglio said.
The technology would be useful for TapImmune’s vaccines, but could also work for infectious diseases or allergies, he noted.
“It’s not only a technology we can use internally, but it’s also something that has out-licensing potential as well, which would be very exciting,” Bonfiglio said.
On the cancer-front, Bonfiglio believes immuno-oncology is the future for treating cancer.
For years people have been using what he calls “blunt force technique,” treatments like radiation and surgery. While he noted that chemotherapy can help, it is also a toxin that has very bad side effects.
“Most people nowadays are not dying from a primary tumor, they’re dying from metastatic disease,” Bonfiglio said.
Being able to not only target and kill the primary tumor, but train the immune system to prevent metastatic disease from happening is how treatment will work, he said.
Bonfiglio likened the future of cancer treatment, to that of HIV. Whereas if you contracted the disease in the 1980s, it was a death sentence, but now it can be treated similar to a chronic disease, with close to a normal life span.
“I believe that’s what is going to happen with cancer in the immuno-oncology area, we’re going to be able to keep cancer from becoming a death sentence and keep it under control with these drugs and the knowledge being used.”
Source: biosciencetechnolgy