 HIV virus possesses inherently complicated nature due to which despite of more than 30 years of efforts, scientists have not yet come up with a reliably effective HIV vaccine.
HIV virus possesses inherently complicated nature due to which despite of more than 30 years of efforts, scientists have not yet come up with a reliably effective HIV vaccine.
There are nine HIV subtypes (called “clades”) in different global populations, according to the World Health Organization. Once the virus enters the body, it can mutate so frequently that it evades the body’s immune response.
“One reason why it’s been so difficult to make an HIV vaccine is that the virus infects the very immune cells that the vaccine should induce,” Guido Silvestri, M.D., chief of microbiology and immunology at Yerkes National Primate Research Center of Emory University in Atlanta, GA, toldDrug Discovery & Development.
HIV invades the body by destroying the immune system’s CD-4 cells, which are necessary to generate antibodies against the virus. The virus mutates and hides in CD-4 cell reservoirs. When these cells multiply to fight an infection, they end up making more copies of the virus.
Scientists are gaining insight into the biology of HIV: they’ve identified certain areas of the virus that don’t change as continuously, making them prime targets for attack by antibodies.
The first trial with successful results

This was the case with the 2009 clinical trial in Thailand. The trial, which included more than 16,000 volunteers, was the largest clinical trial ever conducted for an HIV vaccine — and also the first to show protection against infection.
Two previously developed vaccines, ALVAC-HIV and AIDSVAX, were used in conjunction, with the first initiating an immune response and the second acting as an immunity
booster. The combination, vaccine RV144, reduced HIV risk by a modest 31.2 percent at the end of the three-year study. (Although the vaccine peaked early—it was 60 percent effective at the one-year mark—its effect quickly declined.) Prior to these results, it wasn’t known if a vaccine was achievable.
“My colleagues and I were incredibly excited, almost disbelieving, since the vaccines had not worked by themselves,” Glenda Gray, MBBCH, president of the South African Medical Research Council, told Drug Discovery & Development. Gray, who is based in Johannesburg, directs the Africa Programs for the HIV Vaccine Trials Network (HVTN), the largest worldwide clinical trials network dedicated to the development and testing of HIV/AIDS vaccines. “Soon after, we convened to discuss how we could translate the findings into other parts of the world.”
A promising HIV vaccine in South Africa
South Africa has the world’s highest HIV/AIDS statistic, with an estimated 6.3 million people living with HIV/AIDS. (An estimated 35 million people live with HIV globally.) New infections, called seroconversions, increase at about 370,000 per year in the region—about 1,000 new infections every day.
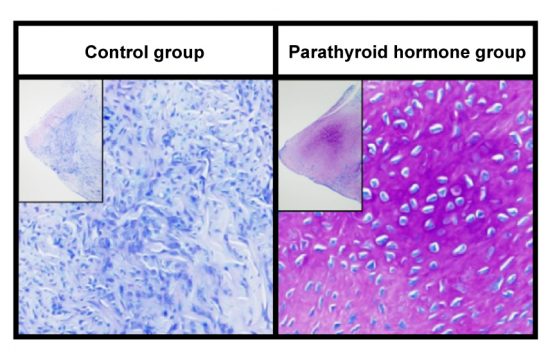
The first in a series of trials designed to build on the success of the Thailand vaccine passed the test: a safety trial using the same vaccine regimen from RV144—but with an added booster shot 12 months afterward, which produced immune responses—triggered the production of CD-4 cells—in healthy adults who received the vaccination. “The durability of the Thai HIV vaccine regimen was not maintained,” Gray told Drug Discovery & Development, “so the idea was to add a more potent adjuvant to the protein part of the regimen, and boost again at 12 months to increase the potency and durability of the regimen.” An ideal HIV vaccine would provide lifelong protection, or at least for a decade.
Sixty-eight of the 100 participants had responses “comparable to or better than those induced in RV144.” The results were presented in late October at the HIV Research for Prevention 2014 conference.
In early 2015, clinical trials began of a modified vaccine tailored to South Africa. An efficacy trial will enroll about 7,000 participants, and results are expected in 2018.
“South Africa has a clade C epidemic, so the first thing we needed to do was make the products clade C specific,” Gray told Drug Discovery & Development. The subtype “C” in South Africa is different than subtypes “B” and “E” found in Thailand. “Now, we are taking the optimized regimen that is clade C-specific with a new protein and adjuvant and are testing this regimen to evaluate whether we can go ahead and do a Phase 3 trial that will lead to licensure.”
How many years might an HIV vaccine take to develop? “It’s an iterative process,” Gray told Drug Discovery & Development. “We don’t know what we don’t know. So we need to take baby steps and learn from trials, and improve the regimen each time.”
Broadly neutralizing antibodies

Antibodies that adhere to the outer envelope, or protein coat, of HIV can inactivate the virus, and potentially stop infection before it begins. An ideal vaccine would produce antibodies that activate all HIV strains. But antibodies against one strain usually don’t work against others.
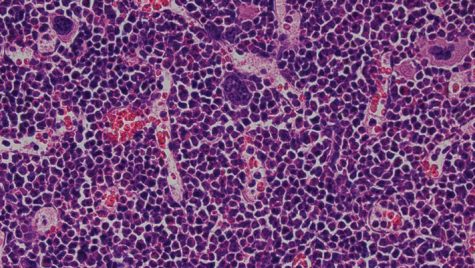
In a breakthrough for HIV vaccines, researchers found that some HIV-infected people naturally produce antibodies that are effective in working against many different HIV strains. These antibodies are called broadly neutralizing antibodies (bnAbs). A problem, though, is that these bnAbs form too late, when people are already infected.
However, since bnAbs can be isolated, scientists can learn about their structure and targets. “This is all very good news,” Silvestri told Drug Discovery & Development. “Not enough, of course, but a good solid scientific foundation to build on.” The goal: todevelop future vaccines that can generate bnAbs before HIV exposure to block HIV infection.
HVTN 104, a Phase 1 clinical trial, will examine the safety and potential of administering bnAbs via injections, and set the stage for subsequent studies. Next up, would be human trials that show that a vaccine can elicit broadly neutralizing antibodies, particularly antibodies that could be maintained for a long period of time.
A different approach
Most recently, scientists at the Scripps Research Institute in Florida found a new method to blocking HIV—with a compound described by Michael Farzan, Ph.D., infectious disease specialist at the institute, as “a potent entry inhibitor” against the virus. The technique worked in non-human primates. The next step, Farzan said, will be to test the compound in infected non-human primates and later, to potentially begin human trials.